- 克利夫兰脐带血中心治疗1型糖尿病的研究
- 来源: 北京市脐血库 时间:2018-04-27
在美国,大约有125万儿童和成年人患有1型糖尿病,每年约有7万名儿童被诊断出患有此病。在发展中国家,这个数字每年增长3%到5%,这表明环境因素的变化可能导致疾病。
1型糖尿病的发病机制
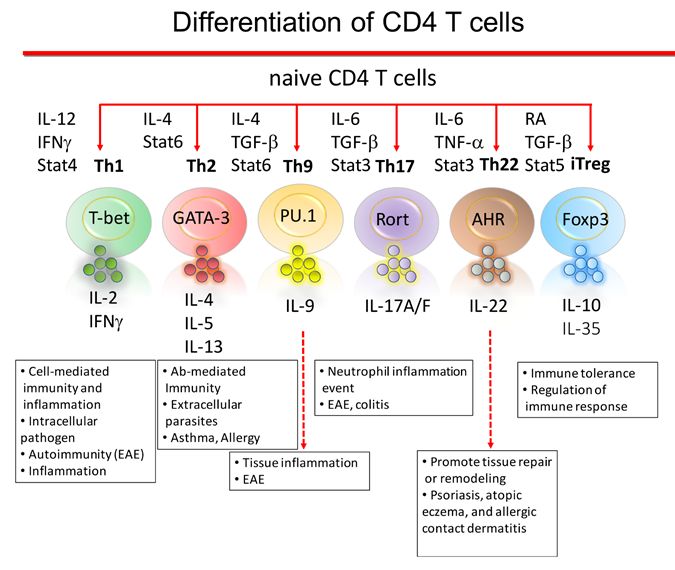
1型糖尿病是由于个人免疫系统破坏胰腺中产生胰岛素的β细胞(胰岛)导致的。当病人被诊断为1型糖尿病时,他们的大部分β细胞已经被破坏了。因此,目前的治疗重点是疾病管理。一个主要的挑战是找出能够重塑免疫反应的治疗方法,从而长期保存β细胞。
患有1型糖尿病的患者血液中调节性T细胞的数量和功能都不正常。调节性T细胞(Tregs)是一种白细胞,是维持耐受和限制自身免疫反应的关键免疫调节成分。
动物研究表明,迁移到炎症区域的Tregs会抑制自身免疫反应。限制Tregs有效治疗1型糖尿病的一个原因是,无法从患病的青少年患者那里获得足够的Tregs。第二个限制因素是,无法在体外生产大量的Tregs同时保持其免疫控制功能的完整。
临床前研究
在克利夫兰脐带血中心(CCBC)的研究人员正在研究健康新生儿脐带血中的T细胞。新生儿的T细胞是独一无二的,因为它们具有很强的T调节能力用于怀孕期间提供婴儿和母亲之间的免疫耐受。
克利夫兰脐带血中心的研究人员正在利用从研究新生儿免疫耐受中获得的细胞生物学知识,并将其应用于治疗1型糖尿病患者。
目前,克利夫兰脐带血中心的研究人员正在进行临床前研究,以证实脐带血中的Tregs能够安全地抑制1型糖尿病患者胰岛细胞所遭受的异常T细胞攻击。当病人最近被诊断时,这种干预预计将是最有效的。如果Tregs能够阻止对患者胰腺中产生胰岛素的胰岛细胞的自身免疫攻击,这将使β细胞恢复,并改善或解决糖尿病问题。
临床研究
最终,克利夫兰脐带血中心的研究人员制定了一种治疗1型糖尿病的方法,具体如下:
筛选一份与1型糖尿病患者配型相合的脐带血单位
从脐血中分离干细胞,并诱导生成Tregs(iTregs);
将iTregs在无菌培养条件下培养三周,以保持T调节功能;
将这些扩增的脐带血iTregs注入到1型糖尿病患者体内。
参考资料:
https://parentsguidecordblood.org/en/news/cleveland-cord-blood-center-research-type-1-diabetes
Cleveland Cord Blood Center Research on Type1 Diabetes
Approximately 1.25 million American childrenand adults have Type 1 Diabetes, with about 70,000 children diagnosed with thedisease each year. That number is rising by 3 to 5 percent annually indeveloping countries, suggesting that changing environmental factors maycontribute to the disease.
Mechanism of Type 1 Diabetes
Type 1 Diabetes is a consequence of theindividual’s immune system destroying the insulin-producing beta cells (islet)in the pancreas. By the time patients are diagnosed with Type 1 Diabetes, amajority of their beta cells have already been destroyed. Hence currenttreatments focus on disease management. A major challenge is to identifytreatments that reset the immune response, and result in long-term beta cellpreservation.
Patients that are developing Type 1 Diabetesdo not have a normal number and function of regulatory T cells in their blood.Regulatory T cells (Tregs) are a type of white blood cell that is a criticalimmune regulator to maintaining tolerance and limiting auto-immune reactions.
Animal studies show Tregs that migrate intoan inflammatory region inhibit auto-immune responses. One limitation to thegeneration of Tregs for effective treatment of Type 1 Diabetes is that very fewTregs that can be obtained from adolescent patients that are developing thedisease. A second limitation is the inability to grow Tregs outside the body togenerate a larger number of cells while keeping their immune control functionintact.
Pre-clinical Studies
Researchers at the Cleveland Cord BloodCenter (CCBC) are studying T cells from the umbilical cord blood of healthynewborn babies. The T cells from newborn babies are unique in that they havevery strong T regulatory capacity in order to provide immune tolerance betweenthe baby and the mother during pregnancy. The CCBC researchers are taking thecell biology knowledge gained from investigating neonatal immune tolerance andapplying it to treat patients with Type 1 Diabetes.
Currently CCBC researchers are conductingpre-clinical studies to verify that Tregs from umbilical cord blood can safelysuppress the abnormal T cell attack on the pancreas islet cells that occurs inType 1 Diabetes patients. It is anticipated that this intervention would bemost effective when the patient is recently diagnosed. If the Tregs can stopthe auto-immune attack on the patient’s insulin-producing islet cells in thepancreas, this will allow beta cell recovery, and improvement or resolution ofthe diabetes. See below for planned clinical trials.
Clinical Studies
Eventually, CCBC researchers envision atreatment approach to Type 1 Diabetes that would proceed as follows:
Identify an umbilical cord blood unit thatis HLA matched to the Type 1 Diabetes patient;
Isolate stem cells from the cord blood unit;Generate induced Tregs (iTregs) from the cord blood stem cells;
Grow the iTregs for three weeks in sterileculture conditions uniquely developed by the research team to maintain Tregulatory function;
Infusethe Type 1 Diabetes patient with these expanded umbilical cord blood Tregs